|
x |
x |
|
 |
 |
|
INFECTIOUS
DISEASE |
BACTERIOLOGY |
IMMUNOLOGY |
MYCOLOGY |
PARASITOLOGY |
VIROLOGY |
|
|
INFECTIOUS DISEASECHAPTER TEN
CENTRAL NERVOUS SYSTEM INFECTIONS
Dr Charles Bryan
Emeritus Professor
University of South Carolina School of Medicine
|
|
|
|
|
|
|
|
Let us know what you think
FEEDBACK |
|

 |
|
TEST YOUR KNOWLEDGE
Bacterial
meningitis
Headache and fever
Acute psychosis
Pneumococcal
pneumonia |
|
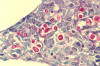
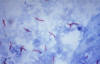
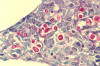
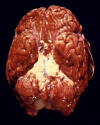 Figure 1
Figure 1
This ventral view of a human brain depicts a purulent basilar meningitis
infection due to Streptococcus pneumoniae bacteria.
Though S. pneumoniae in a normally occurring floral inhabitant of the human
upper respiratory tract, in cases where an individual’s immune system is
compromised, it is responsible for causing paranasal sinusitis, middle ear
infections (otitis media), and lobar pneumonia, as well as meningitis secondary
to these primary respiratory infections. CDC
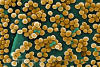
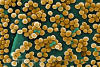
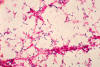 Figure 2
Figure 2
Streptococcus pneumoniae bacteria
grown from a blood culture. Streptococcus pneumoniae, the bacteria
responsible for pneumococcal meningitis, is very common, and normally lives in
the back of the nose and throat, or the upper respiratory tract. CDC
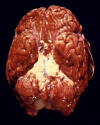
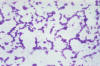
 Figure 3 Figure 3
Aerobic Gram-negative Neisseria meningitidis diplococcal bacteria; Mag.
1150X.
Meningococcal disease is an infection caused by a bacterium called N.
meningitidis or the meningococcus. The meningococcus lives in the throat of
5-10% of healthy people. Rarely, it can cause serious illness such as meningitis
or blood infection. CDC
 Figure 4
Figure 4
Haemophilus influenzae - coccobacillus prokaryote (dividing); causes meningitis in children, pneumonia,
epiglottitis, laryngitis, conjunctivitis, neonatal infection, otitis media (middle ear infection) and sinusitis in adults
(SEM x 64,000)
©
Dennis Kunkel Microscopy, Inc.
Used with permission
 Figure 5
Figure 5
This child has swollen face due to Hib infection.
The tissue under the skin covering the jaw and cheek is infected.
Infection is spreading into her face. She is probably very sick Courtesy of Children's Immunization Project, St. Paul, MN
|
Acute Bacterial Meningitis
Acute bacterial meningitis is a medical emergency variably characterized by
fever, headache, meningismus (stiff neck), nausea, vomiting, and altered mental
status. In about 15% of patients and especially in young children and elderly
patients, the presentation is subtle. Gastrointestinal symptoms may predominate
leading to a misdiagnosis of gastroenteritis. Delayed diagnosis invites tragic
consequences.
The “big 3” causes of community-acquired bacterial meningitis beyond the
neonatal period of life are
Streptococcus pneumoniae,
Hemophilus influenzae type B,
and Neisseria meningitidis. These organisms have in common the ability to
colonize the nasopharynx and to elude host defenses by virtue of their
polysaccharide capsules. Widespread vaccination of young children against H.
influenzae type B now makes this form of meningitis uncommon. N.
meningitidis is a relatively common cause in children, adolescents, and
young adults (See “Meningococcemia” in the chapter on
Sepsis). S. pneumoniae
causes meningitis in all age groups, is the most common cause in older adults,
and is frequent in persons with history of basilar skull fracture.
Listeria
monocytogenes is an important cause in neonates and in patients who are elderly,
debilitated, or immunosuppressed (for example, patients with lymphomas or who
are receiving corticosteroids). Aerobic gram-negative rods are important causes
of meningitis in neonates, elderly patients, and patients who have undergone
neurosurgical procedures.The presentation is, to some extent, age-dependent. Infants may present mainly
with listlessness, poor feeding, and altered breathing patterns. The frail
elderly may present mainly with a decline in the level of awareness. Meningitis
due to Listeria monocytogenes or to aerobic
gram-negative rods usually has a
less dramatic, more sub-acute onset compared to meningitis caused by S. pneumoniae,
H. influenzae type B, or N. meningitidis. When any of the “big
three” cause meningitis in a previously-healthy younger person, the symptoms
usually prompt immediate medical attention. However, the history not
infrequently suggests a nonspecific flu-like illness that gradually worsened
over several days to one week. In this setting, great attention must be paid to
the potential significance of any combination of headache, nausea, and vomiting.
S. pneumoniae is now the most common cause of community-acquired bacterial
meningitis when all age groups are taken into account. Older patients with
pneumococcal meningitis―unlike younger patients with H. influenzae or
meningococcal meningitis―frequently have underlying conditions such as
alcoholism or neurologic disease to which altered consciousness can be easily
attributed. However, patients with pneumococcal meningitis―again, unlike younger
patients with H. influenzae or meningococcal meningitis―frequently have a
clinically-apparent site of infection elsewhere such as
otitis media, sinusitis,
pneumonia, or―rarely―endocarditis.
One should “think meningitis” when patients present with some combination of
fever, headache, stiff neck, nausea or vomiting, and altered consciousness. None
of these symptoms is sufficiently sensitive, however, to exclude meningitis by
its absence. In adults, the overall sensitivity is about 50% for headache and
about 30% for nausea and vomiting. The absence of fever, stiff neck, and altered
mental status allows one to exclude meningitis with 99% to 100% confidence.
Physical examination should target the following areas:
- The skin, looking
for the petechial
rash of
meningococcemia
- The tympanic membranes, looking
for evidence of otitis media as a portal of entry for pneumococcal meningitis
- The optic disks, looking for evidence of
papilledema
as a relative contraindication to lumbar puncture (pulsations in the central
retinal veins effectively exclude increased intracranial pressure)
- Signs of meningeal irritation
Meningeal irritation can be assessed in at least four ways, all of
which can be performed briefly and are therefore recommended:
- Anterior neck flexion. With the patient supine, ask the patient to flex the
head forward (“Put your head on your chest”). Alternatively, ask the patient to
put his or her head between the knees. Neck stiffness is present when the
patient experiences pain on anterior flexion.
- Kernig’s sign: With the patient supine and the hip flexed at 90 degrees, the knee is
extended. Brudzinki’s sign is present when the patient experiences pain or
resistance in the lower back or posterior thigh. This test can also be performed
in the sitting position.
- Brudzinski’s sign: With the patient supine and holding the patient's head,
flex the head so that the chin touches the chest. Brudzinski’s sign is present
when the patient flexes the knees and hips in response to this maneuver.
- The jolt test: Ask the patient to turn his or her head from side to side at a
frequency of 2 to 3 rotations per second. The jolt sign is present when this
maneuver worsens the patient’s headache.
Kernig’s and Brudzinski’s signs have high specificity but low sensitivity for
the diagnosis of meningitis. Jolt accentuation of headache was determined to
have a 97% sensitivity and 60% specificity; in a recent review it was also
concluded that the test has a positive likelihood ratio of 2.2 and a negative
likelihood ratio of zero. It has been suggested that absence of the jolt sign
essentially excludes meningitis. More experience is needed to establish this
point with a reasonable degree of certainty.
When meningitis is suspected, lumbar puncture should be performed. Today’s
frequent tendency to postpone lumbar puncture until a localized intracranial
lesion has been excluded by an imaging study (CT scan or MRI scan) is
unfortunate, because a delay in the institution of therapy of several hours can
be crucial to the outcome. When the illness is acute and there are no localizing
neurologic signs and no evidence of papilledema, the risk-benefit ratio for
lumbar puncture weighs heavily in favor of proceeding with the procedure. Fluid
should be obtained for leukocyte count, differential count, glucose, and protein
content (collectively, these 4 parameters are known as the “CSF formula” and
also for culture. The CSF formula is never diagnostic but can be extremely
helpful, as follows:
- Acute bacterial meningitis: A leukocyte count > 1000/μL with predominance of
polymorphonuclear neutrophils, and with low glucose (< 40 mg/dL or <40% of the
blood glucose) and high protein content (> 150 mg/dL) is highly characteristic.
- Viral (“aseptic”) meningitis: The leukocyte count is usually < 1000/μL with <
50% polymorphonuclear neutrophils on the differential count, with normal glucose
and normal or slightly elevated protein content (exceptions to these rules are
discussed below under “Aseptic Meningitis”).
- Fungal or tuberculous meningitis (chronic meningitis): The leukocyte count is
usually < 500/μL with < 50% polymorphonuclear neutrophils, with low glucose and
elevated protein content.
- Parameningeal infection (such as brain abscess): The leukocyte count is
usually < 1000/μL with < 50% polymorphonuclear neutrophils, normal glucose, and
normal or elevated protein content.
An extra tube of CSF should always be saved, since additional studies may be
indicated if the initial tests are non-diagnostic.
Untreated, meningococcal and pneumococcal meningitis are probably uniformly
fatal. Survivors of H. influenzae meningitis in the pre-antibiotic era often
spent the remainder of their lives in institutions for the severely retarded. |
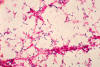
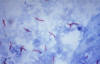
Cryptococcosis of lung in patient with AIDS. Mucicarmine stain.
Histopathology of lung shows widened alveolar septum containing a few
inflammatory cells and numerous yeasts of Cryptococcus neoformans. The inner
layer of the yeast capsule stains red. CDC
|
Aseptic Meningitis, Chronic Meningitis,
and Other Causes of CSF Pleocytosis
There are numerous causes of fever, headache, focal neurologic signs and
symptoms, and CSF
pleocytosis. The more common ones are discussed here because
of the need to distinguish these diverse syndromes and specific diseases from
acute bacterial meningitis.
Aseptic Meningitis (“Viral Meningitis”)
The term “aseptic meningitis” was introduced during the 1930s to describe a
self-limited condition characterized by headache, mild
nuchal rigidity, and
predominantly lymphocytic CSF pleocytosis. The term has been used synonymously
with “viral meningitis,” but it is now recognized that there are many causes of
the aseptic meningitis syndrome including drugs.
Surveillance reports suggest that aseptic meningitis affects about one in 10,000
persons each year; mild cases go unrecognized and the true incidence is unknown.
Rigorous attempts to isolate or identify viruses are successful in the majority
(55% to 70%) of cases. Enteroviruses are by far the most common causes in the
United States (85% to 95% of cases in which a virus is identified). Aseptic
meningitis caused by enteroviruses occurs mainly during the summer and fall.
Infants and young children are most commonly affected. Some of the enteroviruses
can cause a rash. Aseptic meningitis occurs in up to 30% of patients with mumps,
often without evidence of salivary gland disease. The lymphocytic
choriomeningitis virus causes aseptic meningitis with a relatively intense CSF
pleocytosis. This virus is transmitted by rodents such as hamsters, mice, and
rats; hence the disease occurs especially in pet owners, laboratory workers, and
persons living in substandard housing.
Arboviruses such as the St. Louis
encephalitis virus can cause a syndrome resembling aseptic meningitis more than
encephalitis (these terms are relative, since patients with meningitis usually
have some brain involvement and patients with encephalitis usually have some
meningeal involvement). Herpes simplex virus type 2 often causes aseptic
meningitis (in contrast to HSV type 1, which more often causes encephalitis; see
below). Finally, aseptic meningitis is a common manifestation of the acute
retroviral syndrome due to the
human immunodeficiency virus (HIV).
Aseptic meningitis can punctuate the course of many systemic bacterial,
rickettsial, mycoplasmal, spirochetal, and parasitic infections. Aseptic
meningitis occurs in syphilis, especially secondary syphilis. Aseptic meningitis
is a prominent feature of
Lyme disease (neuroborelliosis).
Leptospirosis can
cause an aseptic meningitis syndrome during either or both of the two phases of
the disease: the acute infectious phase or the secondary phase during which
manifestations are presumed due to circulating immune complexes. CSF pleocytosis
can occur during the course of bacterial endocarditis as the result of emboli,
immune-complex encephalitis, or possibly mycotic aneurysm. Drugs are being
reported increasingly as a cause of aseptic meningitis. These include not only
drugs used in chemotherapy (such as azathioprine) but also commonly-used drugs
such as NSAIDs, antimicrobial agents (especially TMP/SMX and its separate
components), ranitidine, and carbamazepine (in patients with underlying
connective tissue diseases).
Onset is usually abrupt with headache and mild nuchal rigidity but the more
severe manifestations of acute bacterial meningitis such as stupor and coma do
not occur.
A presumptive diagnosis of aseptic meningitis can be made when a patient with no
history of recent antibiotic therapy presents with headache and mild nuchal
rigidity and is found to have low-grade CSF pleocytosis, predominantly
lymphocytic, with normal CSF glucose and protein levels. The diagnosis is
confirmed by the clinical course, since a self-limited course distinguishes the
illness from chronic meningitis (e.g., tuberculous meningitis and cryptococcal
meningitis). Problems arise when either the clinical course or the CSF formula
is atypical for aseptic meningitis. Some of the agents of aseptic meningitis
(notably mumps and lymphocytic choriomeningitis) not infrequently cause a low
CSF glucose content.
Occasional patients with aseptic meningitis present with headache, mild nuchal
rigidity, and low-grade CSF pleocytosis with a predominance of polymorphonuclear
neutrophils. When the history and physical examination reveal no other signs or
symptoms pointing to acute bacterial meningitis and when the patient does not
look especially “sick,” the clinician faces a dilemma. Should the patient be
hospitalized and committed to a 7- to 10-day course of treatment for presumed
acute bacterial meningitis? Or should the patient be sent home? A third option
is to observe the patient closely without treatment and to repeat the lumbar
puncture in 4 to 6 hours. The second lumbar puncture reveals CSF with a
predominance of lymphocytes, thus pointing to non-bacterial infection. Recently,
the polymerase chain reaction (PCR) has been shown to be effective for early,
specific diagnosis of enterovirus infection of the CNS.
All patients with aseptic meningitis should be screened for syphilis with a VDRL
on both serum and CSF. It is prudent to save an extra tube of CSF, since at the
time of initial presentation there is always the possibility that the patient
could have one of the causes of chronic meningitis and further studies may be
necessary. Viral cultures of CSF can be attempted, but are unnecessary in daily
practice.
Chronic Meningitis
The term “chronic meningitis” was introduced during the 1970s to embrace a large
number of illnesses causing meningoencephalitis (fever, headache, lethargy,
confusion, nausea, vomiting, stiff neck) and CSF abnormalities (predominantly
lymphocytic pleocytosis, elevated protein, and often low glucose) lasting at
least 4 weeks. Tuberculosis and
cryptococcosis are the most common causes of
chronic meningitis in the United States.
Etiologies are both infectious and non-infectious. The former include
tuberculosis, fungal diseases (cryptococcosis,
coccidioidomycosis,
histoplasmosis,
blastomycosis,
candidiasis, and
sporotrichosis),
spirochetal
diseases (syphilis and Lyme disease),
brucellosis, and parasitic infections (Acanthamoeba
and Angiostrongylus cantonensis). The latter include tumors,
sarcoidosis,
granulomatous angiitis, Behçet’s disease, and uveomeningoencephalitis. Some
patients are given the diagnosis of “chronic benign lymphocytic meningitis,” and
in other cases a satisfactory diagnosis is never reached. Chronic meningitis is
often a component of diseases manifested mainly as encephalitis (for example,
subacute sclerosing panencephalitis due to the measles virus) or as focal
lesions of the CNS (for example, toxoplasmosis).
The onset is typically insidious but can be acute, mimicking bacterial
meningitis or aseptic meningitis. Patients often present with a one- to
several-week history of headache, fever (which can be low-grade), lethargy, and
nausea. If a diagnosis is not made and treatment instituted, the illness
steadily progresses although the course is sometimes characterized by remissions
and exacerbations.
The key to diagnosis of chronic meningitis is early suspicion and lumbar
puncture. An ample volume of CSF should be saved, since a large number of
studies may be necessary. Initial studies of CSF should include cryptococcal
antigen, VDRL, PCR for Mycobacterium tuberculosis, AFB and fungal cultures (each
preferably on 3 to 5 mL of CSF), and cytospin cytology. All patients should also
have a tuberculin skin test, chest x-ray, and imaging of the brain (CT or MRI
with gadolinium enhancement). Additional studies should be targeted on the basis
of a thorough history and physical examination (both of which may need to be
repeated carefully) and the results of initial laboratory tests. For example,
travel or residence in the southwestern United States suggests
coccidioidomycosis; tick exposures in New England or elsewhere suggest Lyme
disease; and eosinophilia in the CSF suggests Coccidioides, parasites, lymphoma,
or chemicals.
Untreated, tuberculous and cryptococcal meningitis are nearly always fatal. In
previously healthy persons, cryptococcal meningitis can cause a subtle,
extremely indolent illness that culminates in dementia. Prognosis for other
forms of chronic meningitis is variable.
Other Causes of CSF Pleocytosis
There are numerous causes of CSF pleocytosis, of which partially-treated
bacterial meningitis is perhaps the most important to the primary care
clinician. Patients who receive oral antibiotics early during the course of
acute bacterial meningitis may show temporary improvement, and the CSF
pleocytosis may shift from predominantly neutrophilic to predominantly
lymphocytic. The CSF protein usually remains high, helping to distinguish this
entity from more benign conditions. The polymerase chain reaction (PCR) may
prove to be highly useful for establishing the diagnosis of partially-treated
bacterial meningitis. Diagnosis of parameningeal infections, discussed further
below, usually hinges on the history, physical examination, and appropriate
imaging studies. Tumors not infrequently cause lymphocytic pleocytosis,
sometimes with low CSF glucose. Seizures sometimes cause mild CSF pleocytosis,
which tends to be predominantly neutrophilic after alcohol-related seizures and
predominantly lymphocytic after seizures caused by stroke. Rare patients
experience recurrent meningitis, the causes of which include leaking cyst
contents from
craniopharyngioma or epidermoid cyst, systemic lupus erythematosus,
and an unusual condition known as Mollaret’s meningitis. Drugs are being
recognized increasingly as a cause of CSF pleocytosis (as discussed in the
previous section on Aseptic Meningitis).
|

H&E-stained micrograph depicting the histopathologic changes seen in brain
tissue due to herpes encephalitis; Mag. 125x.
Characterized by headaches, fever, and altered mental state due to inflammation
of the brain, herpes simplex virus, the cause of HSV encephalitis, is one of the
main causes for non-epidemic, sporadic encephalitis. CDC

A case of a periorbital fungal infection known as mucormycosis, or phycomycosis.
Mucormycosis is a dangerous fungal infection usually occurring in the
immunocompromised patient, affecting the regions of the eye, nose, and through
its growth and destruction of the periorbital tissues, it will eventually invade
the brain cavity.
CDC/Dr. Thomas F. Sellers/Emory University
|
Encephalitis due to Herpes simplex and Other Viruses
Viral encephalitis is a life-threatening process characterized clinically by
altered consciousness and frequently by focal neurologic signs, seizures, and
other abnormalities. Herpes simplex virus, type 1 (HSV-1) is the most important
cause of sporadic viral encephalitis in the United States, although it accounts
for only about 10% to 20% of the estimated 20,000 cases of encephalitis that
occur each year. Prompt diagnosis is crucial since, in contrast to most of the
other forms of viral encephalitis, specific treatment is available.
The major causes of viral encephalitis are the herpes simplex viruses, the
arboviruses,
mumps,
measles, and
varicella-zoster virus.
Encephalitis due herpes simplex virus
About 95% of cases of encephalitis due to herpes simplex virus are caused by
HSV-1, and the remainder by HSV-2. About 70% of these cases result from
reactivation of latent infection and about 30% result from primary infection.
Why occasional patients infected by this common virus develop encephalitis
remains a mystery. Most severely-affected patients are immunologically normal;
indeed an intact immune system may be required for full expression of the
disease since immunocompromised patients tend to have a milder course. There is
little or no evidence for person-to-person transmission or influence by
environmental factors. By contrast, arboviral infections causing encephalitis
are mosquito borne and tickborne.
Viral encephalitis including HSV encephalitis affects persons of all age groups.
Symptoms and signs of HSV encephalitis usually begins suddenly in contrast to
the usual subacute onset of the other forms of viral encephalitis. The first
symptoms sometimes consist of behavioral abnormalities such as hypomania,
elevated mood, and the Kluver-Bucy syndrome (loss of normal emotional responses
such as anger and fear with hypersexuality). Lethargy progresses rapidly to
confusion, stupor, and coma. Fever is usually present and may be high. Herpes
labialis is present in fewer than 10% of cases and its presence or absence has
no diagnostic significance.
The most characteristic symptoms and signs of encephalitis due to HSV-1 are
attributed to the affinity of the virus for the medial temporal and inferior
frontal lobes. This is manifested by some combination of impairment of speech,
bizarre behavior, and olfactory and gustatory hallucinations. Some patients
develop other localizing neurologic symptoms and signs such as
hemiparesis,
ataxia, or cranial nerve palsies. Focal seizures also occur.
Temporal lobe involvement can be demonstrated by imaging procedures (CT or MRI
scan) or by electroencephalography (EEG). MRI scans are more sensitive than and
specific than CT scans especially during the early phases of the disease. The
EEG shows focal abnormalities in more than 80% of cases. Lumbar puncture usually
discloses red blood cells in the CSF, which reflects the necrotizing nature of
the disease. The white cell count, glucose, and protein content in CSF are
variable and occasionally all of these parameters are within normal limits. The
most important specific test on CSF is the polymerase chain reaction (PCR for
HSV-1 DNA). Reported to be up to 98% sensitive and 100% specific, PCR has
replaced brain biopsy as the diagnostic procedure of choice.
Many diseases can mimic herpes simplex encephalitis. These include vascular
disease, brain abscess or subdural empyema, toxic encephalopathy, tuberculosis,
fungal infections (especially cryptococcosis and mucormycosis), tumor, subdural
hematoma, and connective tissue diseases.
The natural history of encephalitis due to HSV-1 was well characterized prior to
the introduction of effective antiviral therapy. Coma developed in about 85% of
patients, seizures in up to 60% of patients, and aphasia in about 20% of
patients. Mortality was about 70% and there was a high prevalence of neurologic
residua among survivors.
West Nile virus infection
West Nile virus, a mosquito-born infection, is probably the best-documented
example of the introduction of a new, vector-borne human infection into the
United States during the twentieth century. The virus is transmitted by at least
29 North American species of mosquitoes that bite both humans and birds—notably corvids (in North America, crows, jays, and ravens; other corvids in Europe are
rooks and magpies). About 20% of humans infected with the West Nile virus
develop a febrile illness, but only about one-half of these patients seek
medical attention. Approximately one in every 150 infected persons develops
meningitis, encephalitis, or both. Advanced age is by far the greatest risk
factor for severe neurologic disease and long-term morbidity. About one-half of
hospitalized patients have severe muscle weakness. Up to 10% of patients have
flaccid paralysis, sometimes suggesting
Guillain-Barré syndrome. The most
efficient method of diagnosis consists of an IgM antibody ELISA testing of CSF
or serum.
|
|
|
Brain Abscess, Subdural Empyema, and Intracranial Epidural Abscess
The term parameningeal infection (literally, “beside the meninges”) encompasses
several syndromes that require prompt diagnosis and, usually, surgical drainage.
Examples include brain abscess, subdural
empyema, septic thrombosis of the dural
sinuses, and epidural abscess (both intracranial and spinal). Newer imaging
studies (CT scan and MRI) simplify the diagnosis.
Brain Abscess
Brain abscess is usually due to spread from a contiguous focus of infection or
hematogenous spread from a distant site of infection. Examples of the former
include sinusitis (mainly frontal and ethmoid), otitis media or mastoiditis,
dental sepsis, and penetrating injury or neurosurgery; examples of the latter
include congenital heart disease with a right-to-left shunt, hereditary
hemorrhagic
telangiectasia with pulmonary arteriovenous fistulas, suppurative
pulmonary infection, endocarditis, and opportunistic infections arising in
patients who are immunocompromised. Brain abscess can also complicate head
trauma. Streptococci, both aerobic and anaerobic, are the usual isolates but
other aerobic and anaerobic bacteria are often present. Unusual microorganisms
such as fungi and
Toxoplasma gondii cause brain abscess mainly in the severely
immunocompromised.
Brain abscess usually presents with some combination of headache, fever, focal
neurologic deficit, nausea or vomiting, seizures, nuchal rigidity, and
papilledema. However, the presenting symptoms often evolve slowly and are
non-specific. Headache is the most common symptom (70% of patients) and can be
localized or generalized. Fever is present in slightly less than one-half of
adults. Altered mental status and hemiparesis are the most common focal
neurologic signs. Neurologic signs frequently predict the site of disease: for
example, bizarre behavior with frontal lobe abscess; speech abnormalities with
temporal lobe abscess; ataxia, nausea, and
nystagmus with cerebellar abscess;
and visual field cuts with temporal, parietal, or occipital lobe abscess.
Symptoms and signs of the predisposing disease such as sinusitis, otitis media,
dental sepsis, or pulmonary disease are often but not always present.
Subdural Empyema
Subdural empyema, which is less common than brain abscess, arises most often
(60% to 70%) as an extension from sinusitis, especially frontal sinusitis.
Otitis media with or without mastoiditis is the other major cause. Cases also
result from trauma or surgery. Streptococci and especially anaerobic
streptococci are again the most common isolates, but staphylococci (notably, S. aureus) and aerobic gram-negative rods are also encountered. Intracranial
epidural abscess, which is rare, has similar predisposing causes and a similar
microbiology.
Subdural empyema usually evolves more rapidly than does brain abscess.
Typically, symptoms suggestive of sinusitis or of otitis media are followed
within days to several weeks by fever, severe headache, neck pain (meningismus)
and then by altered mental status and focal neurologic signs, sometimes with
seizures. Intracranial epidural abscess, on the other hand, usually develops
slowly over weeks or even months. Nonspecific symptoms give way to symptoms of
increased intracranial pressure (nausea, vomiting, headache, altered mental
status) and focal neurologic signs.
The reported mortality for brain abscess now ranges between 0% and 30% and the
mortality for subdural empyema from 6% to 20%. Many patients, and especially
those with subdural empyema, are often left with a neurologic deficit.
|
Methicillin-resistant Staphylococcus aureus bacteria,
commonly referred to by the acronym, MRSA; Magnified 9560x
CDC
Spherical (cocci) Gram-positive Staphylococcus aureus bacteria
magnified 320X
CDC
Mycobacterium tuberculosis bacteria
stained using acid-fast Ziehl-Neelsen stain; Magnified 1000X.
CDC |
Septic Cavernous Sinus Thrombosis
Septic thrombosis of the large dural sinuses that provide venous drainage to the
brain is a rare but life-threatening cause of severe headache. Diagnosis is
usually delayed. There are 3 major syndromes: cavernous sinus thrombosis,
lateral sinus thrombosis, and superior sagittal sinus thrombosis. Here we will
focus on the most common of these syndromes, septic cavernous sinus thrombosis.
Facial infections, most often nasal furuncles, precede about one-half of all
cases of cavernous sinus thrombosis. Sphenoid sinusitis accounts for about 30%
of cases, dental infections about 10% of cases, and the remainder of cases are
originate from otitis media, mastoiditis, or other localized infections. Staphylococcus aureus is the most common etiologic agent and the usual cause of
cavernous sinus thrombosis due to facial infections or sphenoid sinusitis. S. pneumoniae and other streptococci explain some cases, and anaerobic bacteria
sometimes cause the condition especially when it is due to dental infection or
other forms of sinusitis. Diabetes mellitus is possibly a risk factor.
Most patients with cavernous sinus thrombosis present with severe, progressive,
unilateral, retroorbital and frontal headache. The illness usually evolves over
several days but in some cases the headache can be subacute or chronic. Migraine
is a common misdiagnosis. Subsequent symptoms include unilateral swelling of the
orbit, diplopia, and drowsiness. Rapid progression of the disease leads to
proptosis,
chemosis,
papilledema, and ophthalmoplegia (inability to move the
eyeball). Close examination often reveals decreased sensation over the forehead,
nose, upper cheek and lip, and cornea and, on ophthalmoscopic examination,
papilledema or dilated and tortuous retinal veins.
Severe unilateral headache with orbital swelling suggests the possibility of
septic cavernous thrombosis, which then needs to be distinguished from other
conditions. Orbital cellulitis is the most common problem in differential
diagnosis. Other possibilities include
blepharitis, intraorbital abscess,
trauma, tumors (meningioma and nasopharyngeal carcinoma), and several rare
vascular diseases. The CSF is usually but not always abnormal. CSF pleocytosis
is present in about two-thirds of cases and in about one-third of cases the CSF
formula suggests bacterial meningitis (see above). Neurodiagnostic
imaging―currently high resolution CT scan with enhancement or MRI scan with
enhancement―is now the diagnostic procedure of choice.
Untreated, septic cavernous sinus thrombosis is nearly uniformly fatal.
Spinal Epidural Abscess
Spinal epidural abscess classically presents initially with fever and back pain
and progresses to weakness of the lower extremities with impaired bowel or
bladder function and then to paralysis. The correct diagnosis is seldom made at
the first patient encounter.
As seen in primary care practice, spinal epidural abscess is usually a
complication of vertebral
osteomyelitis or
diskitis. Bacteria gain access to the
spine through hematogenous dissemination. Most abscesses are located posterior
to the spinal cord, although below the level of the L1 some of them are anterior
to the cord. S. aureus is the most common microorganism, being found in more
than 60% of cases (>90% of cases in some series), but aerobic gram-negative
rods, streptococci, M. tuberculosis, and other organisms are major causes of the
disease. Spinal epidural abscess also occurs as a complication of spinal
surgery, trauma, drug use, or spinal anesthesia.
Many patients first experience a flu-like illness with fever, malaise,
and―especially if S. aureus is the causative organism―myalgias. As the abscess
expands, patients develop severe, localized back pain often accompanied by nerve
root pain. Weakness in the extremities then develops along with sensory changes
and impairment of bladder or bowel function or both.
Untreated, spinal epidural abscess progresses to complete compression of the
spinal cord with permanent paralysis.
|
|
|
 Return to the Infectious Disease Section of Microbiology and Immunology On-line
Return to the Infectious Disease Section of Microbiology and Immunology On-line
This page last changed on
Tuesday, February 17, 2015
Page maintained by
Richard Hunt
|