|
x |
x |
|
 |
 |
|
INFECTIOUS
DISEASE |
BACTERIOLOGY |
IMMUNOLOGY |
MYCOLOGY |
PARASITOLOGY |
VIROLOGY |
|
TURKISH |
VIROLOGY CHAPTER FOURTEEN
MEASLES (RUBEOLA) AND MUMPS VIRUSES
Dr Margaret Hunt
Professor Emerita
University of South Carolina School of Medicine
|
|
Español |
|
|
|
Let us know what you think
FEEDBACK |
|
SEARCH |
|
|
|

 |
|
Logo image © Jeffrey
Nelson, Rush University, Chicago, Illinois and
The MicrobeLibrary |
|
|
|
TEACHING OBJECTIVES
Brief review of structure
and properties of measles and mumps viruses. Discussion of viral pathogenesis
and disease, epidemiology, prevention and treatment.
|
INTRODUCTION
Infections with measles,
mumps and rubella viruses are confined to man and occur worldwide. They are all
spread primarily via the aerosol route. Each of these viruses exists as a single
serotype. MMR
(mumps, measles, rubella) vaccine contains live,
attenuated forms of all three of these
viruses.
Measles and mumps viruses
belong to the Paramyxovirus Family and are enveloped, non-segmented,
negative-sense RNA viruses with helical symmetry (figure 1A).
|
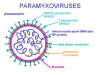
Figure 1A
Paramyxovirus
structure |
PARAMYXOVIRUS FAMILY
The name, paramyxovirus, comes from beyond (para)
and slime (myxo). There are there are two subfamilies of Paromyxoviridae (table
1).
|
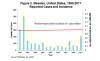
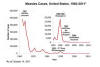 Figure 1B
Figure 1B
Reported cases of measles in the United States 1960-2010
CDC
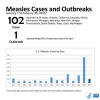
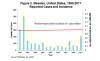 Figure 1C
Figure 1C
Reported cases and incidence of measles in the United States 1995-2011
CDC
 Figure 1D
Figure 1D
Measles cases by import status in the United States 2001-2011
CDC
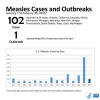 Figure 1E
Figure 1E
Measles cases January 1 to 31, 2015
CDC
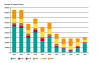
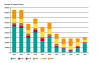 Figure 1F
Figure 1F
Reported measles cases by WHO region, 2005 to 2010. AFR=Africa
AMR=Americas
EMR=Eastern Mediterranean
EUR=Europe
SEAR=South east Asia
WP=Western Pacific
WHO |
MEASLES (RUBEOLA)
Measles (the name is derived from the German word for
blister) is a highly contagious, serious, mainly childhood disease. It was once
widespread in developed countries and remains common in less developed
countries. CDC
estimates that for every 1000 cases of measles, one or two children die and
one quarter of measles cases in the United States require
hospitalization. The disease is so easily spread by water droplets in the air
after a cough or sneeze by an infected person that it is likely that every
non-vaccinated person in that room will contract the disease. Indeed, the
air-borne virus may remain viable for some time.
Epidemiology - Eradication of measles in
the United States by vaccination
Prior
of vaccination, almost everyone got measles and developed childhood
immunity.
In 1941, there were about 900,000 cases of measles in the United States (almost
7000 cases per million population) but as a result of better preventative
measures and better hygiene, the number of cases dropped to around 500,000 per
year by 1960. The attenuated vaccine was introduced in 1962 and within a few
years measles had dropped to around 20,000 cases per year, a 96% reduction (figure 1B, see
here for
further statistics on vaccine effectiveness). In 1981, there were 13,506 measles
cases leading to a recommendation in 1989 for a second booster vaccination.
Cases dropped further to below one per million population (figure 1C) and by
2000, the United States declared the elimination of endemic measles because
almost all cases were shown to be either imported or associated with imported
cases. No endemic measles genotype has been detected in laboratory
analyses in the United States since 1994.
Epidemiology - Resurgence
After the introduction of the second booster shot, endemic measles
was essentially gone from the United States but there was a
small resurgence in 1989-1991. From 2001 to 2011,
there were 904 cases of measles in the United States (37 - 212 cases per year;
median 60). The highest number of cases were in infants who were not old enough
to be vaccinated and about two thirds of the cases were in persons who were
known not to be vaccinated. In 2008, there were 140 cases and almost all of
these were in people who were either unvaccinated or whose vaccination status
was unknown. In 2011, there were 212 cases mostly in people known to be
unvaccinated. Almost all of these 2011cases resulted from infection in Western Europe
which was experiencing a measles epidemic. Indeed, most cases in the 21st
century were import-linked. For example, of the 140 cases in 2008 :
- 25 cases (18%) were directly imported from abroad
- 129 cases (92%) could be shown to be import-associated
For further statistics on import cases, go
here
Epidemiology - 2014 - 2015
The Disneyland-associated cases
There was a record number, 644, of measles cases in the
United States in 2014 and these occurred across 27 states in 23
outbreaks. Many of these cases were associated with cases imported
from the Philippines. In
January 2015, there were 102 cases across 14 states (figure 1E). Almost all of
these cases consist of a single major outbreak linked to Disneyland
in California. Among the cases were five Disneyland employees.
Again, the majority of people who contracted measles were
unvaccinated.
Epidemiology - Worldwide
|
Estimated
number of measles deaths worldwide
(in thousands) 2000 to 2013 |
| 2000 |
535.3 |
| 2001 |
528.8 |
| 2002 |
373.6 |
| 2003 |
484.3 |
| 2004 |
331.4 |
| 2005 |
384.8 |
| 2006 |
227.7 |
| 2007 |
130.1 |
| 2008 |
137.5 |
| 2009 |
177.9 |
| 2010 |
139.3 |
| 2013 |
145.7 |
Measles is still one of the leading
causes of childhood deaths around the world. Before widespread
vaccination outside developed counties, there were 2.6 million
deaths per year (1980 figures). By 2000, this had been reduced to
about half a million (out of over 30 million measles illnesses). Of
these, over 50% were in Arica (figure 1F).
Between 2000 and 2013, global measles
cases fell by 75%, according to WHO. This resulted from more
widespread vaccination and in 2013, 84% of the children in the world
had received the vaccine by their first birthday. WHO estimates that
vaccination prevented 15.6 million deaths between 2000 and 2013.
Nevertheless, in 2013, there were 145,700 deaths worldwide, mostly
in children under 5.
|
|
WEB RESOURCES
Mumps, measles and
rubella vaccine
CDC
Measles, Mumps, and Rubella -- Vaccine Use and Strategies for Elimination
of Measles, Rubella, and Congenital Rubella Syndrome and Control of Mumps: Recommendations of the Advisory Committee on Immunization
Practices (ACIP)
CDC
|
Pathogenesis and disease
(figure
2)
Infection is via an aerosol route (coughs, sneezes) and the virus is very contagious.
Ninety per cent of unvaccinated people who are exposed will become infected. The
virus replicates initially in the upper/lower respiratory tract, followed by
replication in
lymphoid tissues leading to viremia and growth in a variety of epithelial sites.
The disease develops 1 - 2
weeks after infection. Thus, an infected person may not know that he/she is
infected.
Uncomplicated disease is
characterized by the following:
-
Fever of 101 degrees Fahrenheit (38.3 C) or above
-
Respiratory tract symptoms: running nose (coryza) and cough
-
Conjunctivitis (table 2)
-
Koplik's spots on mucosal membranes (table
2) - small
(1 - 3mm), irregular, bright red spots, with bluish-white speck at center. The
patient may
get an enormous number and red areas may become confluent.
-
Maculopapular rash which extends from face to
the extremities. This seems to be associated with T-cells
targeting infected endothelial cells in small blood vessels (table 2).
The infection is
prostrating but recovery is usually rapid. The peak of infectiousness is
during the prodromal phase, that is
before the onset of obvious symptoms (Koplik’s spots, rash). Some virus
shedding continues to occur during the overt disease phase; thus spread of the virus to other
individuals can be somewhat reduced by minimizing contact with others.
The cell-mediated response is important
since patients with
agamma-globulinemia recover normally. Measles tends to be more severe in adults
and the very young (under 5 years of age) and is less severe in older children
and teenagers.
Complications of measles
About 30% of people who are infected by the measles virus
develop some complications such as pneumonia, ear infection or diarrhea.
However, a small number develop much more serious complications.
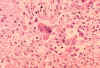
If a patient has an impaired cell-mediated
immune response, there is continued growth of the virus in the lungs leading to giant cell pneumonia (such
patients may not have a rash). This is rare, but often fatal. The reason for the
giant cells is that, since F protein can function at physiological pH, it can
facilitate cell-cell (syncytial) fusion.
Since virus grows in
epithelia of the nasopharynx, middle ear and lung, all of these sites may then be susceptible to
secondary bacterial infection. Otitis media and bacterial pneumonia are quite common.
The outcome of the disease is
affected by the nourishment of the patient and access to medical care. Measles
is still a major killer in underdeveloped countries and several studies in areas
with severe vitamin A deficiency problems have found that vitamin A treatment of
children with measles has resulted in reduction in morbidity and mortality.
Pneumonia accounts for 60% of deaths from measles.
One in 1000 patients may get
encephalitis a few days after the rash disappears. Most patients (90%) survive
encephalitis but there may be complications such as deafness, seizures and
mental disorders.
|
 Figure 2 The pathogenesis of measles. The virus invades the body via blood vessels
and reaches surface epithelium first in the respiratory tract where there are
only 1-2 layers of epithelial cells then in mucosae (Koplik's spots) and finally
in the skin (rash). Adapted from
Mims et al. Medical Microbiology, 1993, Mosby
Figure 2 The pathogenesis of measles. The virus invades the body via blood vessels
and reaches surface epithelium first in the respiratory tract where there are
only 1-2 layers of epithelial cells then in mucosae (Koplik's spots) and finally
in the skin (rash). Adapted from
Mims et al. Medical Microbiology, 1993, Mosby |
| |
Sub-acute
sclerosing pan encephalitis
Very rarely (7 in 1,000,000
cases) the patient may get subacute sclerosing panencephalitis
(SSPE). This develops 1 to 10 years after the initial infection. It is a progressive,
usually fatal, disease and those who survive are severely impaired mentally and
physically. First signs are behavioral, followed by loss of motor control and
coordination. There are jerky movements known as myoclonic seizures. As the
disease progresses speech and swallowing are affected and vision may be
impaired. The course of the disease may be a few weeks although it may also last
for years.
Risk
factors include acquiring primary measles at an early age (usually under two
years). The incidence of SSPE
has decreased
since vaccination against measles was initiated. SSPE is associated with defective forms of the virus in the
brain and so it is difficult to isolate infectious virus from such patients.
Certain
viral proteins are often not expressed, the M protein being frequently absent.
|
Figure
3
A

B
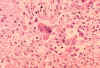 Histopathology of measles pneumonia. Giant cells.
CDC/Dr. Edwin P. Ewing, Jr. epe1@cdc.gov
Histopathology of measles pneumonia. Giant cells.
CDC/Dr. Edwin P. Ewing, Jr. epe1@cdc.gov
C

D

Fusion of Measles Virus Infected Cells. Cell fusion occurring 2 hours
(C)) and 5 hours (D) after infection of a human cell line. Cell nuclei become pyknotic, and by 5 hours, small syncytia fuse into giant ones which show beginning evidence of vacuolation. These syncytia will eventually die and detach from the cell monolayer, leaving behind a visible plaque.
© Linda E. Fisher
University of Michigan - Dearborn
Dearborn, Michigan and The
Microbe Library
|
|
TABLE 2 |
|
CLINICAL ASPECTS OF MEASLES |
|
Site of replication of virus |
Symptoms in a well nourished child with good medical
care |
Symptoms in a malnourished child with poor medical care |
|
Lung |
Temporary respiratory illness |
Pneumonia (life threatening) |
|
Ear |
Otitis media is quite common |
Otitis media is experienced more often and is more severe |
|
Oral mucosa |
 Koplik's spots WHO/Immunization Action Coalition.
Koplik's spots WHO/Immunization Action Coalition.
 Patient who presented with Koplik’s spots on palate due to pre-eruptive
measles on day 3 of the illness
Patient who presented with Koplik’s spots on palate due to pre-eruptive
measles on day 3 of the illness
CDC/Dr. Heinz F. Eichenwald |
Severe ulcerating lesions |
|
Conjunctiva |
 Conjunctivitis: Eyes of child with measles. CDC/Barbara Rice
ber2@cdc.gov
Conjunctivitis: Eyes of child with measles. CDC/Barbara Rice
ber2@cdc.gov |
Severe corneal lesions. There may be secondary bacterial
infections of the eyes and blindness may occur |
|
Skin |
 Maculopapular rash: Face of boy with measles. Third day of rash.
CDC
Maculopapular rash: Face of boy with measles. Third day of rash.
CDC
 Maculopapular rash: This child shows a classic day-4 rash with measles. CDC/NIP/Barbara Rice
Maculopapular rash: This child shows a classic day-4 rash with measles. CDC/NIP/Barbara Rice
 Maculopapular rash:
This child with measles is displaying the characteristic red blotchy
pattern on his buttocks during 3rd day of the rash CDC Maculopapular rash:
This child with measles is displaying the characteristic red blotchy
pattern on his buttocks during 3rd day of the rash CDC
|
Possibility of hemorrhagic rashes (black measles) |
|
Intestinal tract |
No lesion |
Diarrhea which increases malnutrition, halts growth and
impairs recovery |
|
Urinary tract |
Virus in urine |
No further effect |
|
Overall impact |
Serious disease in a small proportion of patients |
Major cause of infant death (estimates of 1.5 million
deaths per year) |
|
Adapted from Mims et al. Medical Microbiology |
|
E

F
 CPE typical of measles virus infection of HeLa cells. The large syncytia, or multinucleated giant cells, result from fusion of cell membranes bearing viral
glycoproteins. Also visible are inclusion bodies, eosinophilic areas of altered staining in the cytoplasm.
Cells stained with hematoxylin, a basic dye, and eosin, an acidic dye.
© Maria-Lucia Rácz, Institute of Biomedical Sciences, University of São Paulo, São Paulo, Brazil
and
The Microbe Library
CPE typical of measles virus infection of HeLa cells. The large syncytia, or multinucleated giant cells, result from fusion of cell membranes bearing viral
glycoproteins. Also visible are inclusion bodies, eosinophilic areas of altered staining in the cytoplasm.
Cells stained with hematoxylin, a basic dye, and eosin, an acidic dye.
© Maria-Lucia Rácz, Institute of Biomedical Sciences, University of São Paulo, São Paulo, Brazil
and
The Microbe Library
G
 Indirect fluorescent antibody serological test for measles virus
immunoglobulin G (IgG) antibody. All cells are counterstained with Evans
blue which fluoresces orange red. Measles virus induces the fusion of
infected cells resulting in a large multinucleated cell (syncytia).
Indirect fluorescent antibody serological test for measles virus
immunoglobulin G (IgG) antibody. All cells are counterstained with Evans
blue which fluoresces orange red. Measles virus induces the fusion of
infected cells resulting in a large multinucleated cell (syncytia).
Kristina M. Obom, Patrick J. Cummings, Maria A.
DeBernardi, Gary Brooker , Johns Hopkins University
and
The Microbe Library
|
Other
consequences of measles infection
Measles can cause
temporary defects in the immune response; for example, tuberculin-positive individuals may
temporarily give a negative response. There may be reactivation of herpes or exacerbation of tuberculosis with natural measles, but this does not seem to
happen with the vaccine strain.
Measles virus replicates in
the cytoplasm, but inclusions containing nucleocapsid protein can also accumulate in the
nucleus. It is not known if this has any effect on the host cell, but histologically
typically giant cells with cytoplasmic and nuclear inclusion bodies are seen
(figure 3). There may also be nucleocapsid protein in the nucleus but the
significance of this is unknown.
Diagnosis
The clinical picture is the first
part of diagnosis; that is exposure
plus upper respiratory tract symptoms, Koplik's spots (table 2) and rash (which is usually
quite characteristic for physicians familiar with measles).
This diagnosis is confirmed by
serodiagnosis,
RT-PCR or isolation. Serodiagnosis by IgG
levels is simpler than isolation but
two
samples are needed, one 10 to 21days post rash, and so takes longer.
There is now also an IgM test. It is recommended that all suspect cases in the United States be confirmed by laboratory testing
Almost all infected
individuals show signs of disease.
There is only one serotype of measles and a single natural infection gives life-long protection. The main route of infection is
via inhalation. Measles virus is highly contagious and the period of maximum contagiousness is
the 2 to 3
day period before onset of the rash.
Prevention
Vaccine
There is an attenuated virus vaccine
that is grown in chicken embryo fibroblast culture.
Current recommendations are to give a first dose of the vaccine at 12 to 15 months.
If given earlier, the recipient does not mount a strong immune
response to the vaccine. A second dose is administered at 4 to 6 years of age, before
the recipient enters
kindergarten or first grade. This reduces the proportion of persons who remain
susceptible due to primary vaccine failure. Students in post-high school
education who do not show evidence of immunity should be given two vaccine
doses 28 days apart.
The vaccine gives long term immunity
and the vaccine virus does not
spread from the vaccinee.
Measles vaccine can cause problems
(e.g. fatal giant cell pneumonia) in those with severely compromised cell-mediated
immunity. No inactivated vaccine is available, due to past problems in which
subsequent infection with naturally acquired measles was sometimes associated
with an atypical, severe form of measles.
The attenuated vaccine has few side effects:
-
Mild fever (1 in 6 vacinees)
-
Mild rash and mild swelling of glands in cheek and neck
(1 in 20)
-
More severe fever
that may cause a seizure (1 in 3000)
-
Temporary joint pain and stiffness (1 in 4)
-
Temporary low platelet count (1 in 30,000)
-
There may be a severe allergic reaction in one in a
million vaccinees
Other problems have been reported after administration of
the vaccine but they are so rare that it is not known if they were the result
of the vaccine or coincidental.
The vaccine is usually given by injection in combination
with vaccines for mumps and rubella (MMR vaccine) and sometimes also with a
varicella vaccine (MMRV vaccine).
Large studies in the United States and Europe have found no
association between the MMR vaccine and
autism.
Why do we need to
vaccinate when measles has been declared eliminated from the United States?
As noted already, all or
almost all cases of measles in the United States are imported. Even in major
developed countries in Europe, there are outbreaks of measles from time to
time in unvaccinated communities. Thus, if we stopped vaccination,
unvaccinated children would still be likely to be susceptible to infection.
Until the disease is eliminated worldwide, vaccination must be maintained.
By having a large fraction of the population immune to measles infection, we
get what is known as "herd immunity" and this protects people in whom the
vaccine has not elicited a sufficient level of immunity and people who
cannot take the vaccine such as very young children and immunocompromized
people.
Herd immunity
If no one were vaccinated (as was the case before 1963), an
infected person would infect anyone with whom he came in contact who had
not already had measles (infection gives life-long immunity). The newly
infected people would infect more and the initial infection in the
community would rapidly become an epidemic. A successfully vaccinated
person will not be infected and will not spread the virus, thus the
disease will spread more slowly. This is the "herd effect". There will
simply be fewer people to pass the virus on from the original patient..
If a very large proportion of the population cannot be infected (as a
result of having already had the disease or because of vaccination), it
is less likely that an infected person will meet a non-immune person to
whom to pass the virus. Thus if the infected person runs the course of
the disease and becomes non-infectious before he or she can infect
another susceptible person, the disease will simply die out. This is
"herd immunity".
|
|
Immune
globulin
Immune serum globulin can
be used for at risk patients during an outbreak; that is those less than 1 year
old or with impaired cellular immunity.
Treatment
No antiviral therapy
available for primary disease. Dehydration should be countered with rehydration
solution and the patient needs good nutrition and fluid intake. Complications should be treated appropriately
such as antibiotics for pneumonia and eye and ear infections. All children in
developing countries who contract measles should be given two doses of vitamin
A, 24 hors apart. This restores low vitamin A levels seen in infected children
and can prevent eye damage. Vitamin A has also been shown to reduce the number
of deaths by 50%.
|
| |
MUMPS
The name comes from the British
word "to
mump", that is grimace or grin. This results from the appearance of the patient as a result
of parotid gland swelling although other agents can also cause
parotitis.
Clinically, mumps is usually defined as acute unilateral or bilateral parotid
gland swelling that lasts for more than two days with no other apparent cause.
Mumps is caused by a paramyxovirus. There is one serotype of the
virus and in an affected patient it can be found in most body fluids
including cerebro-spinal fluid, saliva, urine and blood. The virus can
be grown in cell cultures and in eggs. |
|
WEB RESOURCES
CDC
(requires Acrobat)
Association of State and Territorial Directors of Health Promotion and Public Health Education |
Pathogenesis and disease
Mumps is very contagious and
is probably
usually acquired from respiratory secretions and saliva via aerosols or
fomites.
The virus is secreted in urine and so urine is a possible source of infection.
It is found equally in males and females. Before 1967, most mumps patients were
under 10 years of age but since the advent of the attenuated vaccine, the
remaining cases occur in older people with almost half being 15 years of age or
older.
|
 Figure 4 Pathogenesis of mumps
Adapted from Mims et al Medical Microbiology 1993.
Mosby, 1993
Figure 4 Pathogenesis of mumps
Adapted from Mims et al Medical Microbiology 1993.
Mosby, 1993 |
|
TABLE 3 |
|
CLINICAL ASPECTS OF MUMPS |
| Site of replication of virus |
Symptoms |
Notes |
| Salivary glands |
 Inflammation, parotitis, in a child with mumps. CDC/NIP/Barbara Rice
Inflammation, parotitis, in a child with mumps. CDC/NIP/Barbara Rice
Virus is shed in saliva from 3 days before to 6 days after symptoms |
Salivary gland symptoms are often absent or may be
unilateral |
| Meninges
Brain |
Meningitis
Encephalitis |
Up to 7 days after parotitis |
Meningitis is found in about 10% of cases.
Encephalitis is less common. Usually there is complete recovery;
nerve deafness is a rare complication |
| Kidney |
Virus in urine |
No clinical consequences |
| Testis, ovary |
epididymo-orchitis; rigid tunica albuginea
around testis makes orchitis more painful, more damaging in male |
Common in adults (20% in adult males), often unilateral; not
a significant cause of sterility |
| Pancreas |
Pancreatitis |
Rare complication (There is a possible role in juvenile
diabetes) |
| Mammary gland |
Virus detectable in milk; mastitis in 10%
post-pubertal females |
|
| Thyroid |
Thyroiditis |
Rare |
| Myocardium |
Myocarditis |
Rare |
| Joints |
Arthritis |
Rare |
|
Adapted from Mims et al. Medical Microbiology |
|
 Complications of mumps CDC
Complications of mumps CDC |
Virus infects
upper/lower respiratory tract leading to local replication. The virus spreads to lymphoid tissue
which, in turn, leads to viremia. The virus thus spreads to a variety of sites, including salivary,
other glands and other body sites (including the meninges).
The average time to full
manifestation of disease is 2 - 3 weeks but there may be fever, anorexia, malaise, myalgia
during prodromal phase. Many mumps infections (up to 20%) result in no symptoms
at all and about half of infections result only in the primary respiratory
symptoms.
The symptoms of mumps (figure
4 and table 3) include:
-
Fever
-
Parotitis. Pain from parotitis
swelling persists for 7 - 10 days. This is the most common feature of mumps
and is seen in about 40% of patients. It may be unilateral or bilateral
depending on which salivary glands are infected by the virus.
-
Meningitis. Aseptic meningitis is usually mild.
About three times as many males than females get this . In about half of
patients the meningitis is asymptomatic. In symptomatic meningitis, which
occurs in about 15% of patients, there is stiff neck and headache which
usually resolves in up to 10 days with no further problems.
Mumps-related meningitis is more severe in adults. In very rare cases mumps
can result in encephalitis.
-
Deafness. Mumps was a
leading cause of acquired deafness before the advent of mumps vaccines but
nevertheless hearing loss is rare (one in every 20,000 mumps cases). It is
usually unilateral. The patient may not, in fact, have overt mumps. Deafness may improve with time
but is usually permanent.
-
Orchitis (testicular
inflammation). This is especially
severe in adolescent and adult males and occurs in about 50% of cases.
Sometimes, it occurs along with parotitis. The painful swelling diminishes
after about seven days but tenderness can last for weeks. In 70% of cases,
orchitis is unilateral and results in some degree of testicular atrophy.
Damage tends to be patchy and rarely causes infertility.
-
Pancreatitis. This is an
infrequent side effect of mumps. There is transient hyperglycemia that
resolves. However, there is very little evidence from controlled studies that mumps plays any role in
diabetes mellitus although outbreaks of diabetes have been reported after
mumps outbreaks.
-
Myocarditis. Myocarditis is observed from
electrocardiograms in a minority of patients but is usually otherwise
asymptomatic.
-
Rare complications. These include nephritis, arthralgia (joint
pain) and arthritis (joint inflammation)
Mumps is more severe in
adults and it seems that cell-mediated
immunity is important in recovery. On average, one person dies per year in the
United States now that most people are vaccinated.
|
 Mumps epidemiology CDC
Mumps epidemiology CDC
 Cases of mumps in the United States 1968-2001 CDC
Cases of mumps in the United States 1968-2001 CDC
 Cases of mumps in the United States
1980-2001 CDC
Cases of mumps in the United States
1980-2001 CDC
 Age distribution of mumps cases in the United States 1980-2000 CDC
Age distribution of mumps cases in the United States 1980-2000 CDC
 MMR Vaccine -adverse reactions CDC
MMR Vaccine -adverse reactions CDC |
Diagnosis
Approximately 30% of
infections are sub-clinical.
Parotitis is suggestive as it occurs in 30 - 40% of infections but there are
other causes of parotitis. The disease is confirmed by isolating
the virus, RT-PCR or by
serology. Hemagglutination inhibition, radial hemolysis and complement fixation
assays are rather insensitive. Better is enzyme immunoassay which detects IgM or
IgG. The level of IgM rise during the prodromal phase and peak at about seven
days. Normally, when testing for IgG a specimen is taken during the acute
disease and then during the convalescent phase. The latter should show a higher
antibody titer than the former.
Complement fixing antibody
to the S (soluble) antigen (nucleocapsid protein) is seen for a few months after
infection and is used to diagnose a recent infection. However, one needs to be careful
as there is some cross reaction with other human parainfluenza virus nucleocapsid
proteins. CF antibody to the viral envelope (V antigen) persists.
Epidemiology
Man is the only known natural
host and the disease is found worldwide. There is no 'carrier state'. Since many (about 30%) infections are sub-clinical,
spread is usually via these persons. Mumps is contagious from about 7days
before the infection becomes clinically apparent and continues until about 9 days afterwards.
Until the development of the
highly effective attenuated vaccine, mumps was a very common disease.; for
example, there were 212,000 reported case in the United States in 1964.
Occurrence dropped to about 3,000 cases by the mid 1980's which is about one
case per 100,000 population. In 2001, there were 231 United States cases. In
1986/87, there was a jump in mumps in people in the 10 - 19 years age group
(12,848 cases) which was attributable to the fact that these people were born
before routine immunization. Vaccine failure may also have contributed.
From time to time, outbreaks of mumps still occur, often in the
winter or spring in crowded environments such as schools and colleges. In 2011
to 2013, there were outbreaks on college campuses in the United States in
California, Virginia and Maryland but these were limited in extent. In
2009-2010, there were approximately 3,000 cases in a single outbreak among
school children in a religious community in New York. The center of the epidemic
was one child who had contracted mumps in the United Kingdom during an outbreak
there.
Prevention
The
attenuated vaccine virus, which is made in chick embryo fibroblasts, does
not spread to contacts and gives long-term immunity (greater than 95% efficacy
with immunity lasting more than 25 years). It is usually given as MMR vaccine
that contains three live,
attenuated viruses: mumps, measles and rubella. It is also
available as a single virus preparation or combined with the rubella vaccine.
Normally, two doses separated by four weeks are recommended for children more
than one year of age.
Vaccine is contraindicated in
immunosuppressed patients and in pregnant women, although there is no evidence
that the vaccine can damage the fetus. Also people who have severe allergic
reactions after a previous mumps vaccination should not receive the MMR vaccine.
The virus is rapidly inactivated by organic solvents such as
chloroform and ether (as would be expected of enveloped viruses) and also by UV light and formaldehyde.
Treatment
There is no specific
treatment for mumps.
MMR VACCINE AND AUTISM
There have been reports in the media linking autism to
administration of the MMR vaccine. These were the result of a small study (12
children) by Dr Andrew Wakefield and his colleagues in London who suggested that
the vaccine caused inflammatory bowel disease. This allowed proteins to enter
the circulation that would otherwise not be there and which could then move to
the brain and cause neurological damage. Larger studies have failed to establish
such a link and the original paper has been retracted.
Among the findings in such studies reported by CDC (link)
are:
-
There is no indication that measles vaccine contributes to
the development of long-term neurological damage, including educational and
behavioral deficits
-
There is no difference in the prevalence of autism among
children born before the introduction of the MMR vaccine in Sweden and those
born after the vaccine was introduced
-
In a 1999 study of 498 children with autism in the UK, it
was found that the age at which they were diagnosed was the same regardless
of whether they received the MMR vaccine before or after 18 months of age or
whether they were never vaccinated. The first signs or diagnoses of autism
were not more likely to occur within time periods following MMR vaccination
than during other time periods. Also, there was no sudden increase in cases
of autism after the introduction of MMR vaccine in the UK. Such a jump would
have been expected if MMR vaccine was causing a substantial increase in
autism.
|
|
WEB RESOURCES
Facts about autism
CDC
Facts about MMR vaccines and autism
CDC See also:
The MMR-autism
scare
- our story so far
|
|
 Return to the Virology section of Microbiology and Immunology On-line
Return to the Virology section of Microbiology and Immunology On-line
 Return to the Home Page of Microbiology and Immunology On-line
Return to the Home Page of Microbiology and Immunology On-line
This page last changed on
Sunday, October 30, 2016
Page maintained by
Richard Hunt
|

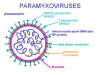
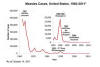 Figure 1B
Figure 1B Figure 2 The pathogenesis of measles. The virus invades the body via blood vessels
and reaches surface epithelium first in the respiratory tract where there are
only 1-2 layers of epithelial cells then in mucosae (Koplik's spots) and finally
in the skin (rash). Adapted from
Mims et al. Medical Microbiology, 1993, Mosby
Figure 2 The pathogenesis of measles. The virus invades the body via blood vessels
and reaches surface epithelium first in the respiratory tract where there are
only 1-2 layers of epithelial cells then in mucosae (Koplik's spots) and finally
in the skin (rash). Adapted from
Mims et al. Medical Microbiology, 1993, Mosby
 Histopathology of measles pneumonia. Giant cells.
CDC/Dr. Edwin P. Ewing, Jr. epe1@cdc.gov
Histopathology of measles pneumonia. Giant cells.
CDC/Dr. Edwin P. Ewing, Jr. epe1@cdc.gov

 Figure 4 Pathogenesis of mumps
Adapted from Mims et al Medical Microbiology 1993.
Mosby, 1993
Figure 4 Pathogenesis of mumps
Adapted from Mims et al Medical Microbiology 1993.
Mosby, 1993 Complications of mumps CDC
Complications of mumps CDC Mumps epidemiology CDC
Mumps epidemiology CDC