|
x |
x |
|
 |
 |
|
INFECTIOUS
DISEASE |
BACTERIOLOGY |
IMMUNOLOGY |
MYCOLOGY |
PARASITOLOGY |
VIROLOGY |
| |
CHAPTER NINETEEN - HEPATITIS
PART ONE - DISEASE TRANSMITTED ENTERICALLY
HEPATITIS A AND E
Dr Richard Hunt
Professor
Department of Pathology, Microbiology and Immunology
University of South Carolina School of Medicine
|
|
EN
ESPANOL -
SPANISH |
| |
| |
| |
|
Let us know what you think
FEEDBACK |
|
SEARCH |
|
|

 |
|
Logo image © Jeffrey
Nelson, Rush University, Chicago, Illinois and
The MicrobeLibrary |
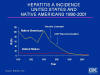
 Figure 1
Figure 1
Acute Viral Hepatitis by Type, United States, 1982-1993
CDC |
The five viruses described in Chapter Eighteen cause
hepatitis. "Infectious hepatitis" is caused by hepatitis A virus (HAV); "serum
hepatitis" results from hepatitis B virus (HBV) and the delta agent (HDV).
"Non-A, non-B hepatitis" is caused by hepatitis E (HEV) and hepatitis C (HCV)
viruses (figure 1). HAV and HEV are transmitted
enterically, while HCV, HBV
and HDV are transmitted
parenterally. There are more than 700,000 cases of
viral hepatitis per annum in the United States, of which more than half are
asymptomatic. Despite the availability of highly effective vaccines against
hepatitis A and hepatitis B, these diseases are among the most reported
vaccine-preventable diseases in the United States.
|
Virus |
A |
B |
C |
D |
E |
G |
| Disease |
Infectious hepatitis |
Serum hepatitis |
Non-A, non-B hepatitis
Post transfusion hepatitis |
Delta agent |
Enteric non-A, non-B
hepatitis |
|
| Source |
Feces |
Blood and body fluids Sexual contact |
Blood and body fluids Sexual contact |
Blood and body fluids Sexual contact |
Feces |
Blood and body fluids |
| Transmission |
Enteric Fecal-Oral |
Parenteral Percutaneous
Permucosal |
Parenteral Percutaneous
Permucosal |
Parenteral Percutaneous
Permucosal |
Enteric Fecal-Oral |
Parenteral Percutaneous
Permucosal |
| Sexual transmission |
Yes (especially homosexual) |
|
|
|
|
|
| Chronic infection |
No |
Yes |
Yes |
Yes |
No |
Yes |
| Incubation period |
15 - 20 days |
45 - 160 |
14 - 180 |
15 - 64 |
16 - 60 |
? |
| Carcinogenesis |
No |
Hepatocellular carcinoma |
Hepatocellular carcinoma |
Hepatocellular carcinoma |
No |
? |
| Cirrhosis |
No |
Yes |
Yes |
Yes |
No |
? |
| Severity of disease |
Usually mild. Very low mortality |
Sometimes severe 1 -2% mortality |
Usually (80%) asymptomatic Up to 4%
mortality |
Super-infection with HBV - often very
severe with high mortality rate Co-infection with HBV - often severe |
Usually mild except in pregnancy |
Asymptomatic to mild |
| Prevention |
Vaccine |
Vaccine |
Behavior Modification Blood
screening |
Behavior Modification HBV vaccine |
Safe water No vaccine |
|
| Chemotherapy |
|
|
Peginterferon/ Ribovirin |
|
|
|
| United States chronic infections
(total) |
None |
1- 1.25 million |
3.5 million |
70,000 |
None |
|
| United States acute infections per
year (estimated) |
125,000 to 200,000 |
140,000 to 320,000 |
35,000 to 180,000 |
6,000 to 13,000 |
|
|
| United States Deaths per year from
fulminant hepatitis |
100 |
150 |
? |
35 |
None |
? |
| United States Deaths from chronic
liver disease |
None |
5,000 |
8,000-10,000 |
1,000 |
|
|
|
 Figure 2
Figure 2
Hepatitis A virus
CDC |
INFECTIOUS HEPATITIS - HEPATITIS A VIRUS
Hepatitis A virus (HAV) (figure 2) causes infectious hepatitis which is transmitted via
the oral-fecal route as a result of close contact such as in day-care
centers. The virus is also spread by sexual contact and in contaminated
food. Rarely (in fewer than 1% of cases) is HAV spread by blood
products, blood transfusions or intravenous drug use.
This form of hepatitis accounts for about 40-50% of all hepatitis cases
(figure 1). The
orally ingested virus first enters the bloodstream via the lining of the
intestinal tract and then migrates to the liver parenchymal cells. These
cells become infected because they have the immunoglobulin-like HAV cellular
receptor on their surfaces. The virus replicates rather slowly and is shed into the bile and passed in the stool. The symptoms of HAV
and HBV are very similar. There is only one HAV serotype worldwide and
humans are the only reservoir.
|
| |
Symptoms
The most obvious symptom is jaundice. HAV also causes abdominal pain, nausea
and diarrhea. In addition, the patient may suffer fatigue and fever. Chronic
infections with HAV do not occur but some patients may experience symptoms
for up to 9 months.
|
| |
Carcinogenesis
There is no evidence for HAV being the cause of liver cancer (hepatocellular
carcinoma).
|
 Figure 3
Figure 3
Events in hepatitis A infection CDC |
Immune response
Virus particles are found in the bloodstream from three days to five weeks
after infection and in the stool from one to five weeks after infection. In
the latter part of this period, raised liver enzymes in the bloodstream
(e.g. alanine amino transferase) are observed. IgM (which is used in
diagnosis) rises soon after the initial infection and peaks at about 5
weeks. Anti-HAV IgG rises later (two to three weeks) (figure 3). There is a cytotoxic T
cell and natural killer cell response that kills infected cells. The humoral
response is also important in counteracting the virus but most pathological
effects of the virus are the result of the immune response rather than the
virus itself. Once the patient has cleared the virus, the anti-HAV IgG antibody response
gives life-long protection.
|
 Figure 4
Figure 4
Concentration of HAV in various body fluids CDC |
Pathology
There is a prodromal (incubation) phase of between two and eight weeks after
infection, following which there is an abrupt onset of symptoms. After about two weeks of infection, virus is detectable in the
liver, blood and stool (Feces can contain up to 108 infectious
virions per milliliter and are the primary source of HAV) (figure 4). The virus replicates in hepatocytes but little
cellular damage ensues. Thus, the symptoms of infectious hepatitis are not
caused by the presence of HAV in the liver but by the immunological response
of the host to its presence. Initially, patients experience fatigue, pain in
the abdomen and nausea and there are elevated levels of liver enzymes in the
serum
A few days after the first symptoms, jaundice (icteric symptoms) often
occurs; this is particularly noticeable in the sclera. Jaundice is seen in
about 60% of adults but far fewer children (up to 20%). There is also dark
urine and light stool. Children show lesser symptoms than adults; for
example, jaundice is seen among fewer than 10% of children younger than 6
years of age, 40%-50% of older children and 70%-80% of adults.Almost all
(99%) patients make a complete recovery within two to four weeks with no
chronic sequelae. In about 0.1% of patients, fulminant hepatitis occurs
leading to death in the majority of these patients (about 50-80%). This results
from liver failure and encephalopathy. Other rare complications are
relapsing hepatitis and
cholestatic hepatitis (in which there are very high
bilirubin levels). The former, which has
symptoms similar to the original infection, usually occurs within three
months of the initial HAV infection. In cholestatic hepatitis, liver damage
by the virus occurs leading to obstruction of bile secretion. This is most
often seen in immuno-compromised patients.
|
 Figure 5
Figure 5
Risk factors for hepatitis A in United States CDC
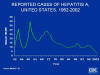
 Figure 6A
Figure 6A
Reported Hepatitis A Cases, By Year Northern Plains Indian Reservation,
South Dakota, 1968-2002 CDC
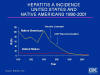 Figure 6B
Figure 6B
Incidence of hepatitis A in American Indians 1990-2001 CDC
|
Epidemiology
The incidence of HAV infection in the United States has fallen from about 12
cases per 100,000 population in the 1980ís to 2.9 in 2002 (figure 7B). This is largely
due to the availability of the vaccine. In 2001, there were 93,000 new HAV
infections in the United States. There were an estimated 45,000 acute
clinical cases (but many fewer were actually reported). in the United
States, hepatitis A outbreaks used to occur in 10 to 15 years cycles.
Since transmission is via the oral-fecal route, members of the family of an
infected person are most at risk. Community outbreaks are common but in half
of all cases no risk factor is identified (figure 5). The infected person is contagious
before overt symptoms appear. Many infected persons are asymptomatic (most
children and up to a half of infected adults) but still shed infectious
virus. In addition, conditions of poor housing and cramped conditions lead
to spread of the virus. There are frequent outbreaks in daycare centers that
are then transmitted to other family members. The virus is also transmitted
as a result of sexual contact, especially homosexual sex and, since it is
blood-borne, can be spread by sharing needles during use of intravenous
drugs. The virus is very resistant to a variety of agents including low pH,
organic solvents and detergents. It is also resistant is temperatures as
high as 61 degrees for 20 minutes. Besides direct fecal-oral transmission
(such as by contaminated hands), the virus may be spread in contaminated
drinking water and where raw sewage is present since the virus can survive
for months in fresh or salt water. Particularly problematic is sewage
contamination of oysters and other shellfish that are filter-feeders. In
developing countries, most people get mild HAV infections as children and
then retain life-long immunity. Approximately 30% of the population of the
United States is seropositive with a much higher incidence in third world
countries.The highest rates of hepatitis A in the United States are found
in Hispanic and Native American populations (figures 6, 7D). The lowest are among Asian
Americans. This undoubtedly reflects socio-economic conditions such as
crowding and also contact with persons from countries such as Mexico with
high HAV infection rates. These factors result in higher hepatitis A
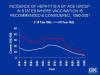
incidence in western states (figure 7A, G, H). In 1990, hepatitis A incidence was highest in
children (figure 7C) with about an equal male to female ratio; however, by 2001, the
gender/age incidence had changed markedly with the highest incidence in
young to middle aged men (figure 7 I, J). This is because the incidence of hepatitis A has
fallen as a result of vaccine use and HAV is now mainly spreading among
intravenous drug users and homosexual men.
The virus is found worldwide with the highest levels in under-developed
countries (figure 7E). In underdeveloped countries, nearly all children have anti-HAV
antibodies indicative of a prior infection and epidemics are rare. In
countries with higher levels of sanitation, infection occurs in older
individuals and clinical disease is more often seen; very often there are
localized outbreaks. In some countries with high hygiene standards (e.g.
Scandinavia), clinical disease outbreaks are again rare and hepatitis A is
seen primarily in intravenous drug users.
|
Figure 7
A.
Distribution of hepatitis A in the United States by county CDC |
 B.
Reported cases of hepatitis A in the United States 1952-2002 CDC
B.
Reported cases of hepatitis A in the United States 1952-2002 CDC
 C.
Incidence of hepatitis A by age group 1990-2001 CDC
C.
Incidence of hepatitis A by age group 1990-2001 CDC
 D.
Incidence of hepatitis A by race in United States CDC
D.
Incidence of hepatitis A by race in United States CDC
 E.
Global distribution of hepatitis A CDC
E.
Global distribution of hepatitis A CDC
 G.
Hepatitis A incidence in United States. Comparison of 1987 - 97
average with 2002 CDC
G.
Hepatitis A incidence in United States. Comparison of 1987 - 97
average with 2002 CDC
 H.
States with highest hepatitis A rates CDC
H.
States with highest hepatitis A rates CDC
 I.
Hepatitis A in the United States by age and gender 1990 CDC
I.
Hepatitis A in the United States by age and gender 1990 CDC
 J. Hepatitis A in the United States by age and gender
2001 CDC
J. Hepatitis A in the United States by age and gender
2001 CDC
|
 F.
Hepatitis A Incidence, United States,
F.
Hepatitis A Incidence, United States,
1980-2002 |
| |
Diagnosis
An ELIZA test for anti-HAV IgM is available. Diagnosis is also made from the
symptoms and the clusters of cases that occur. The presence of IgG within
the first few weeks of infection suggests a prior infection or vaccination.
|
| |
Treatment
There is no treatment. Supportive care should be given. Hepatitis A immune
globulin can be administered early after infection (two weeks) and gives
some temporary immunity (up to five months).
|
| |
Control
Improved hygiene is the most important factor in stemming the spread of HAV.
Chlorination of water is very effective. Before the present vaccine, passive
immunity was obtained using immune gamma globulin which was effective
against the disease in most cases if given before infection as prophylaxis
or during the early incubation period. The present very effective vaccines (HAVRIX
and VAQTA) used in the United States are killed (formalin) virus preparations. The
vaccine is given in the first year of life and immunity, probably life-long,
results within a month. In adults, the vaccines give protective immunity
within one month of vaccination in most recipients. A second dose leads to
100% protection.
|
| |
There is a combined anti-HAV/HBV vaccine approved in the United States for
recipients of 18 years and older. It contains Hepatitis A antigen and HBsAg.
In other countries, this vaccine is available for children.
|
| |
ENTERIC NON-A, NON-B HEPATITIS
- HEPATITIS E |
 Figure 8
Figure 8
Geographic distribution of hepatitis E CDC |
Hepatitis E virus (HEV) causes enteric non-A,
non-B hepatitis and is transmitted via the oral-fecal route through
contaminated drinking water. It is not usually transmitted directly from one
patient to another (in contrast to HAV). HEV outbreaks can be extensive and
is likely the cause of much of the acute sporadic hepatitis seen in areas
where the virus is found (figure 8). In countries of low incidence, HEV infections are
usually seen in travelers.
After an incubation 16 to 60 days (with an average of 40 days), typical
hepatitis symptoms arise (jaundice, malaise, abdominal pain, nausea etc).
Virus may be excreted in the stool for several weeks after the onset of
symptoms. There is no evidence for chronic HEV infections but persistence in
the population may be the result of a low level of infections between
epidemics. In pregnant women the mortality rate is high.
|
 Figure 9
Figure 9
Hepatitis E infection - Typical serologic course CDC |
Immunology
After a prodromal phase of about a month, symptoms occur. Virus is found
earlier in the stool . Alanine aminotransferase rises at the same time anti-HEV
IgM and IgG. By about two months, elevated alanine aminotransferase
diminishes, as does IgM. IgG remains and results in short term immunity
(figure 9).
Diagnosis
There are no commercially available tests for routine diagnosis
|
| |
Epidemiology
HEV is endemic to many tropical countries where good sanitation is lacking.
In the United States less than 2% of the population has anti-HEV antibodies.
The source of these infections is not known.
Prevention
Possibly contaminated drinking water should be avoided as should uncooked
food in endemic areas. Immune globulin is not effective if it comes from
donors in western countries. There is no vaccine.
|
|
 Return to the Virology section of Microbiology and Immunology On-line
Return to the Virology section of Microbiology and Immunology On-line
This page last changed on
Friday, February 05, 2016
Page maintained by
Richard Hunt
|

 Figure 1
Figure 1 Figure 2
Figure 2 Figure 3
Figure 3 Figure 4
Figure 4 Figure 5
Figure 5
 D.
Incidence of hepatitis A by race in United States CDC
D.
Incidence of hepatitis A by race in United States CDC G.
Hepatitis A incidence in United States. Comparison of 1987 - 97
average with 2002 CDC
G.
Hepatitis A incidence in United States. Comparison of 1987 - 97
average with 2002 CDC I.
Hepatitis A in the United States by age and gender 1990 CDC
I.
Hepatitis A in the United States by age and gender 1990 CDC F.
Hepatitis A Incidence, United States,
F.
Hepatitis A Incidence, United States, Figure 8
Figure 8 Figure 9
Figure 9